WHAT IS INFLAMMATION?
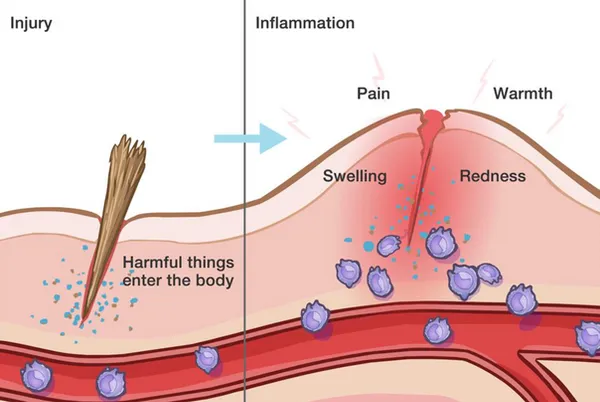
Inflammation is a protective mechanism of the body, triggered by something it perceives to be a threat. When the body encounters something it considers invasive or dangerous (like viruses, bacteria, or toxic chemicals), it activates the immune system. The immune system sends out its first responders: inflammatory cells and cytokines (substances that stimulate more inflammatory cells). This also occurs when there is an injury to the body, and the immune system activates to send repairing agents to the area.
These cells begin an inflammatory response to trap bacteria and other offending agents or start healing injured tissue. The result can be pain, swelling, bruising or redness. Imagine a baseball hits someone in the leg, then a few hours later that area is swollen. This is a simple example of the immune system activating the process of inflammation.
In some conditions, like autoimmune diseases, the immune system acts as if regular tissues are infected or somehow unusual, sounding the alarm constantly and continuously creating inflammation. This leads to chronic inflammation, and can be a very challenging situation.
CAN INFLAMMATION OCCUR IN THE BRAIN?
This question is important to consider when recovering from a brain injury, and is actually paramount to a successful recovery. The answer is a resounding YES. A brain injury creates inflammation in the brain, known as neuroinflammation, that can lead to secondary injuries, severe lingering symptoms, and a slower recovery process.
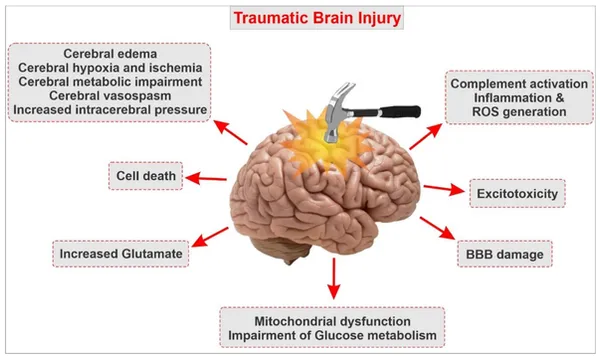
Now that you know the basics of inflammation, we can apply this understanding to a traumatic brain injury (TBI). When a blow to the head occurs, there is a series of events that follows, creating a cascade of inflammation in the brain, or neuroinflammation.
WHAT IS NEUROINFLAMMATION AND WHY IS IT PREVENTING MY TBI RECOVERY?
Neuroinflammation can be simply described as inflammation that occurs in or around the brain. Many things can cause neuroinflammation, such as:
For the rest of this article, however, we will be focusing on how traumatic brain injury (TBI) leads to neuroinflammation. TBI causes physical damage to the central nervous system with accompanying neurological dysfunctions. While this may seem obvious given the traumatic circumstances of the event, the notable component of these symptoms is that they can last indefinitely, despite the brain’s ability to repair itself over time.
Before we explain the process of neuroinflammation and the neuroinflammatory cascade that follows a brain injury, let’s first discuss the blood-brain barrier.
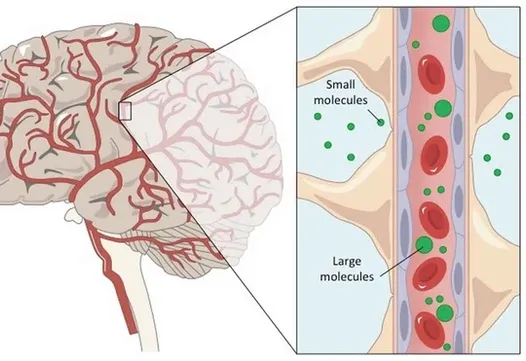
The brain is precious, and evolution has gone to great lengths to protect it from damage. The most obvious is our 7mm thick skull, but the brain is also surrounded by other protective mechanisms.
One important protective element is the blood–brain barrier. The blood-brain barrier is a thin lining that surrounds the brain and is designed to allow only nano-sized particles in or out as needed. As the name suggests, this is a barrier between the brain’s blood vessels (capillaries) and the cells and other components that make up brain tissue. Whereas the skull, meninges and cerebrospinal fluid protect against physical damage, the blood–brain barrier provides a defense against disease-causing pathogens and toxins that may be present in our blood.
However, like the gut, it can become damaged and “leaky,” allowing foreign invaders in. One of the biggest risks to triggering brain inflammation is a leaky blood-brain barrier.
HOW DOES A TBI CAUSE NEUROINFLAMMATION?
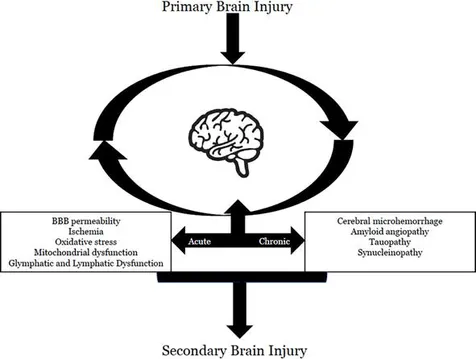
A traumatic brain injury (TBI) creates a cycle of neuroinflammation that can lead to secondary injuries and symptoms.
This is a brief overview of the neuroinflammatory cascade following a TBI:
LEAKY GUT SYNDROME AND NEUROINFLAMMATION
A typical human body is designed to take in a variety of foods, which are sent through different parts of the gastrointestinal system (i.e. digestive system) to be processed and converted into energy. Beneficial nutrients are absorbed and sent to the rest of the body for nourishment, while harmful components (toxins) are filtered out and excreted.
But what happens if the lining of the gastrointestinal tract or stomach is damaged, causing harmful toxins to enter the bloodstream? This is what we call Leaky Gut Syndrome (or intestinal permeability), and it is quite common after brain injuries.
With Leaky Gut Syndrome, undigested food particles cross into the bloodstream, resulting in inflammation and impaired nutrient absorption.
These undigested particles trigger a severe immune reaction, as the immune system sends signaling molecules and cytokines to the area, resulting in inflammation. Perhaps the most troubling part of Leaky Gut is that these cytokines are even capable of crossing the blood-brain barrier, which can cause inflammation in the brain–what we call neuroinflammation.
When the brain becomes inflamed, there is a drastic reduction in brain activity and this can majorly limit one’s ability to recover from a TBI, stroke, or concussion. This even has an impact on the gut-brain connection, which can create further issues in digestion. Basically, it is a loop of inflammation that needs to be broken.
Healing the gut lining becomes a top priority in this case, and resources like Cavin Balaster’s How To Feed A Brain can help along with your doctor’s recommendations.
REDUCING NEUROINFLAMMATION AND RESTORING THE BLOOD-BRAIN BARRIER
Because neuroinflammation occurs at acute and chronic stages after the primary insult in TBI, a treatment targeting neuroinflammation may have a wider therapeutic window for TBI. We focus on ways of reducing inflammation and preventing further neuroinflammation through our therapies, IV treatments, and nutritional guidance.
Although the blood-brain barrier degrades easily, it can also regenerate through dietary and lifestyle modifications similar to how you can repair leaky gut. For instance, high stress degrades the blood-brain barrier, but normalizing stress can allow it to repair. Simply stabilizing your blood sugar and stress levels, removing inflammatory foods, addressing chronic health issues, and taking powerful antioxidants can help restore the blood-brain barrier.
Common symptoms of neuroinflammation:
Supplements/herbs known to reduce neuroinflammation:
To learn more and become a patient at Resiliency, please fill out this contact form.
Research:
Neurofeedback Therapy is emerging as a promising treatment modality known to positively impact conditions such as PTSD, anxiety, depression, concussion / post-concussion syndrome (PCS), stroke, and TBI (traumatic brain injury). It has also been shown to improve attentional deficits, learning disabilities, and other cognitive impairments.
We currently do not offer neurofeedback therapy here at Resiliency, though we understand it is gaining interest in the field. Many of our patients have asked about it since it is becoming quite popular and entering the mainstream, so we wanted to offer some information about what it is. The concept of self-regulation discussed in this article is particularly relevant to our patients, as we utilize this approach when teaching our patients how to regulate their nervous systems during and after treatment.
What is Neurofeedback Therapy?
Neurofeedback Therapy is essentially a method for retraining the brain toward more desirable thought patterns and brainwave states. This happens through a feedback loop involving a computer-brain interface that provides real-time positive and negative feedback to the patient.
Neurofeedback is a type of biofeedback, which means certain information and metrics about physiological functions are being recorded in real-time during the therapy.
Neurofeedback, rather than involving heart rate, blood pressure, or skin temperature like other types of biofeedback, focuses solely on brain activity.
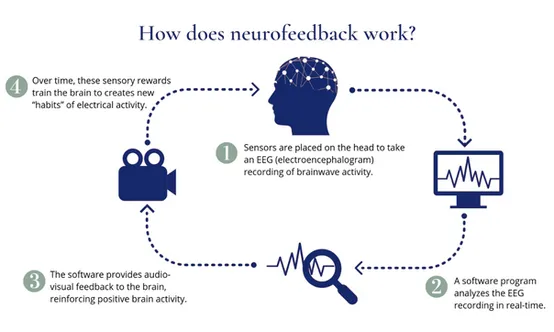
The patient wears an EEG cap that contains sensors placed at specific points around the head. These sensors detect and measure electrical activity across the various brain regions, sending live data to the computer interface.

The computer program will then begin directing the client’s brainwave activity toward more desirable and controlled patterns through visual and auditory cues. They’ll get immediate feedback from the program when their brainwave patterns improve to reinforce those changes.
The idea is that patients can see their brain waves depicted in front of them. If they can learn to shift their thoughts to produce a desired pattern of activity, they can solve the harmful effects associated with the original pattern of activity.
What Are Brainwaves / Brainwave States?
The brain has billions of neurons, and each individual neuron connects (on average) to thousands of others. Communication happens between them through small electrical currents that travel along the neurons and throughout enormous networks of brain circuits. When all these neurons are activated they produce electrical pulses – visualize a wave rippling through the crowd at a sports arena – this synchronized electrical activity results in a brainwave, or brainwave state.
When many neurons interact in this way at the same time, this activity is strong enough to be detected even outside the brain. By placing electrodes on the scalp, this activity can be amplified, analyzed, and visualized. This is electroencephalography, or EEG.
One way that EEG brainwaves convey information is in their rate of repetition. Some oscillations, measured on the scalp, occur at more than 30 cycles per second (and up to 100 cycles per second) These cycles, also called frequencies, are measured as Hz or hertz. These brainwaves are typically lower frequency and slower when sleeping, and higher frequency and faster while awake and alert.
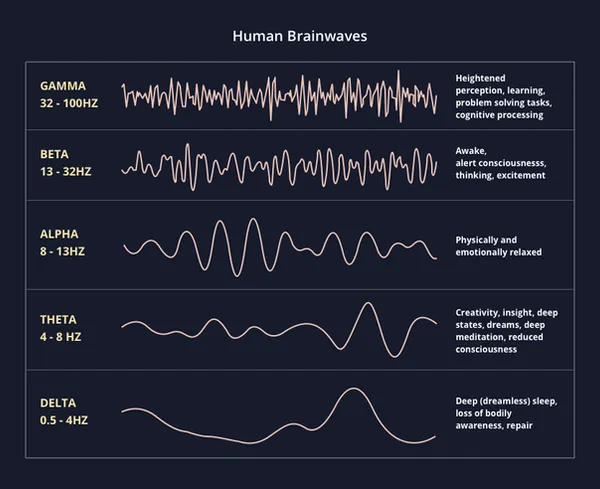
Overview of the Different Brainwave States
There have been 5 different brainwave states recorded through EEG. In order from slowest to fastest, these are: delta, theta, alpha, beta, gamma.
Delta (0.5 - 4 Hz)
During deep, restful sleep, the brain is in a delta state. This is when the brain and body can repair and heal the best. This is the slowest brainwave state.
Theta (4 - 8 Hz)
Theta is known to be the state associated with dreaming (whether daydreaming or during sleep), deep relaxation, and even creativity. Theta states have been recorded more in the brains of advanced meditators.
Alpha (8 - 13 Hz)
When in an alpha state, one feels relaxed yet fully present, allowing emotional and physical relaxation to occur. This is a meditative state where one feels completely calm, and we shift into alpha before we fall asleep.
Beta (13 - 32 Hz)
The majority of one’s active day will likely be spent in a beta state, which is the state of thinking, excitement, and stress. Being stuck in a beta state when trying to relax can be difficult and leads to chronic stress, however. Balance is important.
Gamma (32 - 100 Hz)
Gamma is the state of peak performance, high level problem solving, learning, and heightened cognitive activity.
The Importance of Self-Regulation
A major aspect of neurofeedback’s benefits is the concept of self-regulating brain activity. Brain injuries and conditions such as PTSD make self-regulation significantly more difficult, meaning that a stimulus can trigger a state of heightened sympathetic (fight-or-flight) activity, and it feels nearly impossible to calm down and switch back into parasympathetic (rest-and-digest).
The inability to self-regulate often occurs for our patients due to underactivity in one’s frontal lobe, which is the part of the brain meant to essentially “put the brakes'' on repetitive negative thought patterns, among its other functions.
Decreased activity in the frontal lobe and impaired frontal lobe connections are common in many cases of post-concussion syndrome, TBI, PTSD, depression, and anxiety, so we see learning self-regulation as a necessary part of a successful recovery.

For example, many people with PTSD experience heightened activity in their amygdala (fear center) due to an impaired connection between the amygdala and frontal lobe. The frontal lobe is meant to calm the amygdala and allow the person to feel relaxed in their environment, but if that connection is damaged, the signals cannot be sent effectively, leaving the individual constantly scanning their surroundings for threats and feeling on-edge.

We can develop self-regulation as a skill by strengthening the frontal lobe’s connections to other parts of the brain through deliberate, consistent practice of neurofeedback, meditation, and other exercises.
Through neurofeedback therapy, one can recognize more quickly when they are in a stressful, hyperactive brain state such as high beta, and be able to use slow, deep breathing or other learned methods to switch into a more calm alpha state.
This ability is invaluable when recovering from a brain injury or mental health condition, as well as in general for living a human life with the resilience to overcome challenges.
Research suggests that neurofeedback therapy can be particularly effective when combined with other self-regulation exercises such as mindful breathing, humming, gargling water, and other practices known to activate the vagus nerve. These methods can empower the individual to cultivate more resilience and stability as they navigate life.
Conditions That May Benefit from Neurofeedback Therapy
While neurofeedback research is ongoing and ever-growing for a range of conditions due to the promising impacts, the following have been studied enough to show consistent benefit:
To become a patient at Resiliency, please fill out this contact form.
WHAT IS COLD LASER THERAPY?
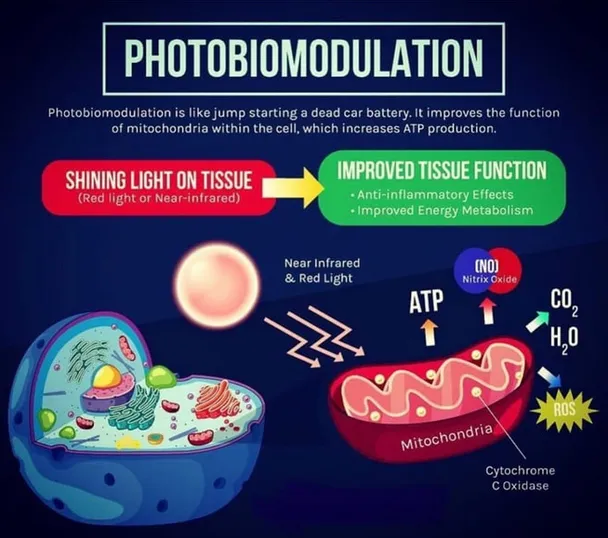
Cold Laser Therapy, often known as Low-Level Laser Therapy (LLT), is a well-researched therapeutic modality that utilizes light to generate cellular energy, reduce inflammation, and promote rapid healing. This occurs through a process called photobiomodulation (PBM), which will be described in detail later in this article.
Cold Laser Therapy, or LLLT, began as a medical treatment in 1967, originally used for pain relief and wound healing. As researchers and clinicians observed the anti-inflammatory and regenerative properties of low-level laser therapy, the medical applications of LLLT have broadened to include conditions such as stroke, myocardial infarction, and degenerative or traumatic brain disorders.
Many of the most compelling applications of LLLT are in the field of neurology (both central and peripheral). Many serious brain diseases and injuries can be successfully treated with noninvasive transcranial laser therapy. Furthermore, in the peripheral nervous system, LLLT can be used effectively for nerve regeneration and pain relief.
HOW DOES COLD LASER THERAPY WORK?
Cold Laser Therapy utilizes a process called photobiomodulation, where light is converted into usable cellular energy. Biological reaction to light is nothing new, as there are numerous examples of light induced photochemical reactions in biological systems. Vitamin D synthesis in our skin is an example of a photochemical reaction. Our vision is based upon light hitting our retinas and creating a chemical reaction that allows us to see. Throughout the course of evolution, photons have played a vital role in photo-chemically energizing certain cells.
In simple terms, the light penetrates the skin and enters the cells, where it is absorbed and converted into energy. Mitochondria in the cells contain chromophores which are the principal photoreceptors that absorb the light. The light energy is utilized to generate more adenosine triphosphate (ATP) for cellular use. In addition, the process creates mild oxidants (ROS), which leads to gene transcription and then to cellular repair and healing.
The process also unclogs the chain that has been clogged by nitric oxide (NO). The nitric oxide is then released back into the system. Nitric oxide is a molecule that our body produces to help its 50 trillion cells communicate with each other. This communication happens by transmission of signals throughout the entire body. Additionally, nitric oxide helps to dilate the blood vessels and improve blood circulation.
WHAT IS BRAIN PHOTOBIOMODULATION?
Brain Photobiomodulation is a light therapy that uses red to near-infrared (NIR) light to stimulate, heal, and protect tissue in the brain that has been injured or is at risk of dying. In this example of a research study conducted on the use of photobiomodulation for treating sports-related concussions, increased brain volumes, improved functional connectivity, and increased cerebral perfusion and improvements on neuropsychological test scores were observed.
The brain is the most important and complex human organ. Within every brain cell are mitochondria, which are best understood as energy-producing “powerhouses” or “batteries”. Through biochemical reactions, the mitochondria create fuel for brain cells.
Your brain’s mitochondrial performance can be improved by absorbing light energy (photons) of specific wavelengths through photobiomodulation. Scientific research shows our brain’s mitochondria respond positively to light energy within the red and near infrared (NIR) wavelength range.
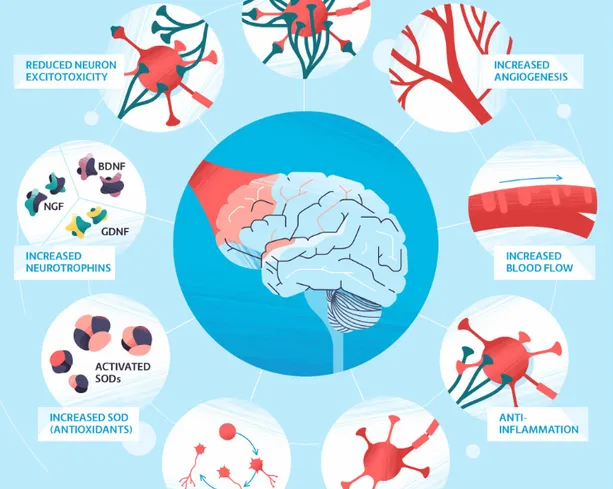
Collectively, brain photobiomodulation heals damaged brain cells, improves cerebral blood circulation, reduces inflammation and toxicity, and regenerates damaged brain cells. In a nutshell, red or NIR light energy to the brain improves efficiency and performance due to better signaling and repaired connectivity between the neurons.
Research and clinical studies show that when NIR light energy has sufficient power density, it is capable of penetrating biological tissue and bone to produce therapeutic outcomes without negative side effects.
BENEFITS OF COLD LASER THERAPY
The benefits of cold laser therapy, or low-level laser therapy (LLLT), for brain injuries can be categorized into two main areas of function.
Boosting Cellular Metabolism:
Through the process of photobiomodulation, cold laser therapy can provide a significant boost to the energy efficiency and metabolism of cells. For many of our patients with neurological deficits, we can direct the cold lasers to the specific lobes of the brain or parts of the brain stem that are underfunctioning. This has been shown to increase neuronal activity and upregulate those areas of the neuraxis that have been damaged.
Reducing Inflammation:
The cascade of neuroinflammation that results from multiple head traumas is a major obstacle to healing. Cold laser therapy has been shown to reduce inflammation in the brain, as well as in the GI tract and joints.

CONDITIONS THAT MAY BENEFIT FROM COLD LASER THERAPY
– Traumatic Brain Injury (TBI)
– Post Concussion Syndrome (PCS)
– Stroke
– Depression
– PTSD
– Anxiety
– Parkinson’s
– Alzheimer’s
– Other neurodegenerative disorders
– Spinal cord injury
– Edema
The literature on cold laser therapy is growing rapidly. Currently, there are over 220 published studies on cold laser therapy and brain photobiomodulation.
To become a patient at Resiliency, please fill out this contact form.