The autonomic nervous system (ANS) is a network of neural pathways that controls various organ systems in the body in order to maintain homeostasis. These functions are involuntary, meaning the ANS functions without conscious control. You can think of autonomic like “automatic.”
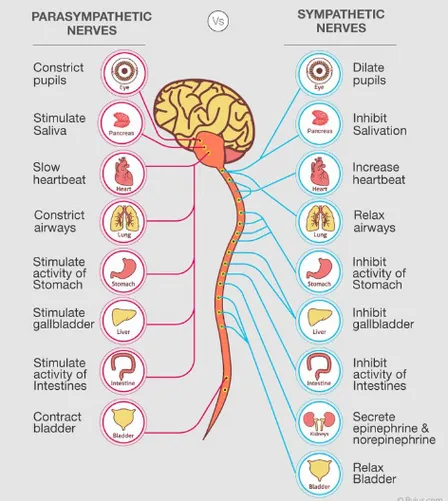
The autonomic nervous system is comprised of two systems: the sympathetic nervous system (fight-or-flight) and the parasympathetic nervous system (rest-and-digest).
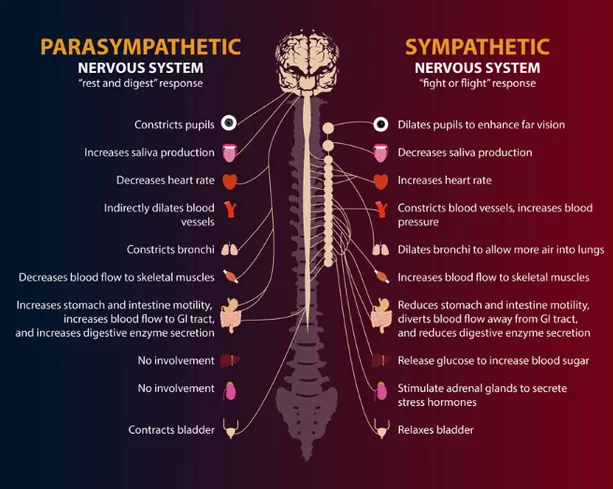
These two systems control different bodily functions, utilize different neurotransmitters (chemicals used to communicate), and follow different paths through the body. The sympathetic nervous system carries signals that put your body’s systems on high alert, while the parasympathetic nervous system carries signals to relax those systems. The balance here is crucial, as we will explore below.
When recovering from a concussion, traumatic brain injury (TBI), or stroke, it is important to understand the balance between these two systems, as an imbalance can seriously inhibit recovery.
The sympathetic nervous system[1] is a network of nerves that is activated during stressful or dangerous situations, as well as during physical exercise. When you are in a stressful or dangerous situation, your sympathetic nervous system activates and causes a “fight-or-flight” response, which means your heart rate and blood pressure rise, your pupils dilate (enlarge), your gut stops digesting food to divert energy elsewhere, and you feel hyper alert.
While this is certainly beneficial and necessary in some circumstances when we need to act quickly, it should not be our baseline throughout the majority of the day, as we will discuss later in this article.
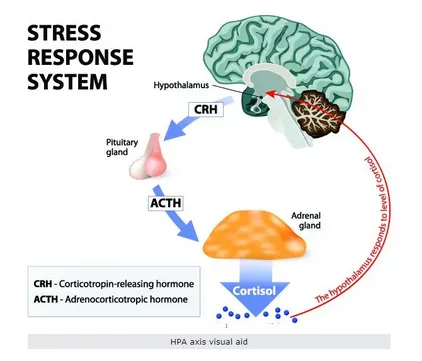
A key area of the sympathetic nervous system that is particularly relevant to concussion, TBI, PTSD, and stroke patients is the hypothalamic-pituitary-adrenal (HPA) Axis. The HPA Axis, as its name suggests, is a complex feedback system involving the hypothalamus and the pituitary gland in the brain, and the adrenal glands on top of the kidneys.
Simply put, stress[2] causes the body to release stress hormones into the bloodstream. First, the hypothalamus receives a message from the amygdala (fear center in the brain) that stress is present. The hypothalamus releases corticotropin-releasing hormone (CRH) and arginine vasopressin (AVP), which then tell the pituitary gland to produce adrenocorticotropic hormone (ACTH) and release it into the bloodstream. When this ACTH reaches the adrenal glands, this signals the adrenal glands to produce cortisol[3], commonly known as the “stress hormone.”
Feedback is sent upstream to the hypothalamus when sufficient corticosteroids are detected in the blood, signaling that the hypothalamus can stop producing CRH and AVP to then slow the production of cortisol. However, when living in chronic psychological stress or after a brain injury, this feedback loop can be disrupted, leading to a consistently elevated amount of cortisol in the blood.
It is important to note here that stress can mean physical stress such as extreme cold or extreme heat, as well as psychological stress. We have included a section below describing different types of stress, and how some forms are actually beneficial for the nervous system and body.
The nervous system is the central organizing system within the body, and brain injuries have the potential to drastically impact the feedback system in the HPA Axis due to damage to the frontal lobe and an overactive amygdala.
The amygdala is the fear center of the brain, responsible for processing fear, arousal, and emotional stimuli to determine the appropriate response. The amygdala is typically kept in check by the frontal lobe, which is known as the inhibitory lobe, as it can “apply the brakes” on other parts of the brain. One of the frontal lobe’s jobs is to process the information from the amygdala and determine whether a stimulus is a threat or not.
The frontal lobe is often affected by brain injuries and concussions, so its ability to calm the amygdala is severely impaired. This leads to an inaccurate perception of environmental threats, perpetuating the release of stress hormones and essentially being stuck in “fight-or-flight” mode.
Research[4] shows a strong correlation between an overly active HPA Axis (sympathetic overdrive) and suicidal ideation, as the stress diminishes the frontal lobe’s executive function ability.
Cortisol, while labeled as the “stress hormone”, certainly does have important functions in the body. Cortisol levels are meant to fluctuate throughout the day, following our body’s natural rhythms. For example, cortisol levels are meant to be higher in the morning upon waking, and lower at night when going to sleep.
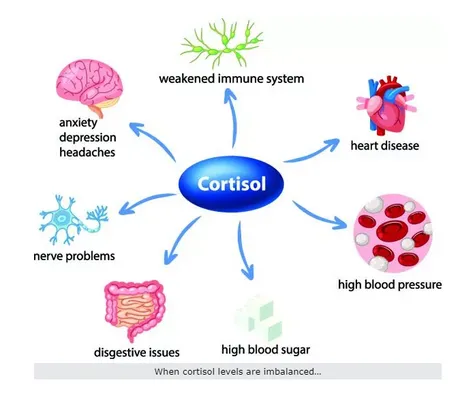
However, as mentioned above, many people struggle with a constant state of low-level stress, leading to an unhealthily high level of cortisol in their blood for sustained periods.
Symptoms of high cortisol levels:
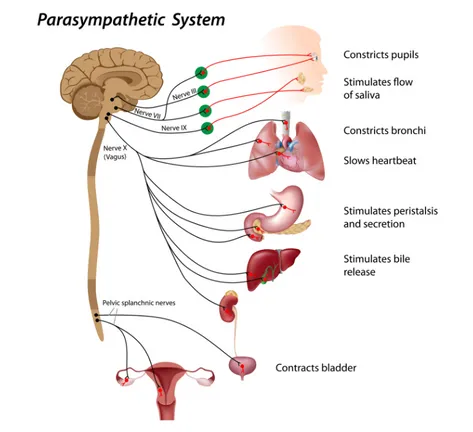
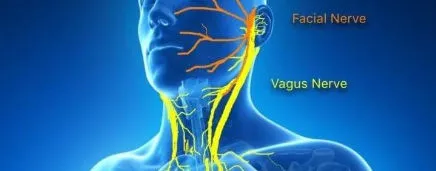
The parasympathetic nervous system is a network of nerves that relaxes your body and allows life-sustaining processes, like digestion, during times when you feel safe and relaxed. The vagus nerve makes up about 75% of the parasympathetic nervous system overall, connecting to your heart, lungs, and other vital organs all the way down to your bladder and bowels.
BALANCE IS KEY
Autonomic nervous system imbalances and disorders can arise for many reasons and present in different ways. People with too much sympathetic activation and too little parasympathetic activation experience tense, stressed, anxious states of mind with little to no ability to relax. On the other hand, those with too little sympathetic activation and too much parasympathetic present as apathetic and depressed with little to no motivation.
The connection between autonomic nervous system imbalance and cognitive decline is currently being explored[5]by researchers, suggesting that even middle aged adults can experience significant cognitive decline from an overactive sympathetic nervous system.
SYMPATHETIC OVERDRIVE AND PARASYMPATHETIC DYSREGULATION
Much of the signaling for the parasympathetic system originates in the brain stem and is therefore highly susceptible to disruption resulting from an impact such as a motor vehicle accident or blast injury. This causes many of our patients to experience an underactive parasympathetic nervous system[3], meaning their overall ANS balance is skewed significantly toward sympathetic and are essentially stuck in fight-or-flight.
Sympathetic overdrive, as it is often called, presents as a range of symptoms including heightened anxiety, chronic stress, constipation, indigestion, emotional instability, tachycardia (increased heart rate), and hypertension (high blood pressure).
“GOOD STRESS” AND “BAD STRESS”
“Good stress”, known as hormetic stress, actually creates resilience in the brain and body and serves a very important role throughout the course of one’s life. Exercise is the most common hormetic stressor, so here we will use the example of lifting weights. The exercise of lifting weights creates stress on the muscles involved, which ultimately strengthens them. You may feel heightened energy and alertness (fight-or-flight) when pushed to your limit physically, but eventually should settle back down into parasympathetic where recovery takes place.
Within the last few decades, researchers have been interested in exploring the correlations between overall health and the regular practice of hormetic stress practices that involve deliberately putting the body into extreme conditions, such as cold plunging and sauna, for short periods. The research is promising, though please consult your doctor before beginning any of these practices. We mainly bring these practices up to demonstrate the concept of a hormetic stressor: a controlled, deliberate practice that puts stress on the body, with a clear ending to the stress.
The “bad stress” is the chronic, constant feeling of stress that many people feel as their baseline throughout their lives.
The challenge lies with our cultural acceptance of feeling stressed all the time, believing that being chronically stressed is simply the norm. Long, stressful workdays, empty consumption, and fruitless pursuits keep many of us living in a constant state of fear and stress. This kind of stress, chronic stress, is quite detrimental to overall health and puts people at risk for a number of diseases and disorders.
THE BRAIN NEEDS PARASYMPATHETIC FOR RECOVERY
We explained the detrimental effects that high cortisol levels have on the body, and these tend to be intensified by the body’s inability to switch into parasympathetic “rest-and-digest” mode.
When the brain is stuck in fight-or-flight, it is difficult for any recovery to take place, as the nervous system is unable to fully relax and allow the body’s energy to be used for healing and recovery. Therefore, a major component of many TBI and concussion recovery protocols is parasympathetic activation, i.e. improving one’s parasympathetic tone, through the vagus nerve.
DYSAUTONOMIA
Dysautonomia is the umbrella term for when one’s autonomic nervous system does not function properly, several examples of which we have mentioned throughout this article. Aside from traumatic brain injuries and concussions, many people (about 70 million worldwide) suffer from dysautonomia. Dysautonomia can stem from many causes, not only brain injuries:
To become a patient at Resiliency, please fill out this contact form.
Research:
2 Stress-induced activation of the sympathetic nervous system
3 Neuroanatomy, Parasympathetic Nervous System
5 Parasympathetic and sympathetic nervous systems interactively predict change in cognitive functioning in midlife adults
6 Physiology, Cortisol