WHAT IS INFLAMMATION?
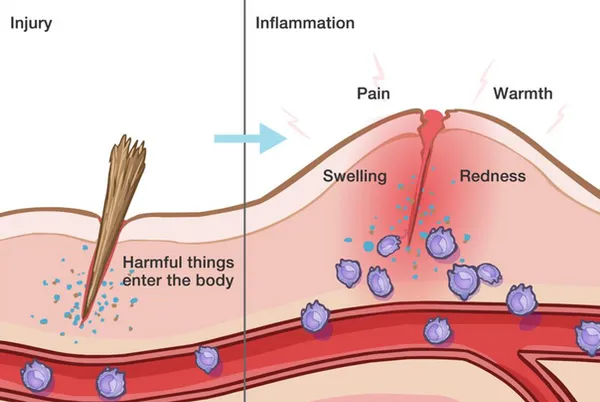
Inflammation is a protective mechanism of the body, triggered by something it perceives to be a threat. When the body encounters something it considers invasive or dangerous (like viruses, bacteria, or toxic chemicals), it activates the immune system. The immune system sends out its first responders: inflammatory cells and cytokines (substances that stimulate more inflammatory cells). This also occurs when there is an injury to the body, and the immune system activates to send repairing agents to the area.
These cells begin an inflammatory response to trap bacteria and other offending agents or start healing injured tissue. The result can be pain, swelling, bruising or redness. Imagine a baseball hits someone in the leg, then a few hours later that area is swollen. This is a simple example of the immune system activating the process of inflammation.
In some conditions, like autoimmune diseases, the immune system acts as if regular tissues are infected or somehow unusual, sounding the alarm constantly and continuously creating inflammation. This leads to chronic inflammation, and can be a very challenging situation.
CAN INFLAMMATION OCCUR IN THE BRAIN?
This question is important to consider when recovering from a brain injury, and is actually paramount to a successful recovery. The answer is a resounding YES. A brain injury creates inflammation in the brain, known as neuroinflammation, that can lead to secondary injuries, severe lingering symptoms, and a slower recovery process.
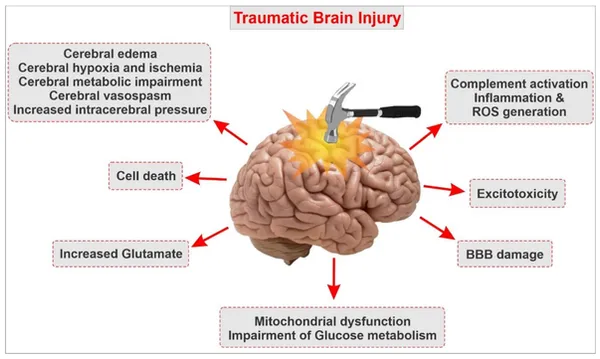
Now that you know the basics of inflammation, we can apply this understanding to a traumatic brain injury (TBI). When a blow to the head occurs, there is a series of events that follows, creating a cascade of inflammation in the brain, or neuroinflammation.
WHAT IS NEUROINFLAMMATION AND WHY IS IT PREVENTING MY TBI RECOVERY?
Neuroinflammation can be simply described as inflammation that occurs in or around the brain. Many things can cause neuroinflammation, such as:
For the rest of this article, however, we will be focusing on how traumatic brain injury (TBI) leads to neuroinflammation. TBI causes physical damage to the central nervous system with accompanying neurological dysfunctions. While this may seem obvious given the traumatic circumstances of the event, the notable component of these symptoms is that they can last indefinitely, despite the brain’s ability to repair itself over time.
Before we explain the process of neuroinflammation and the neuroinflammatory cascade that follows a brain injury, let’s first discuss the blood-brain barrier.
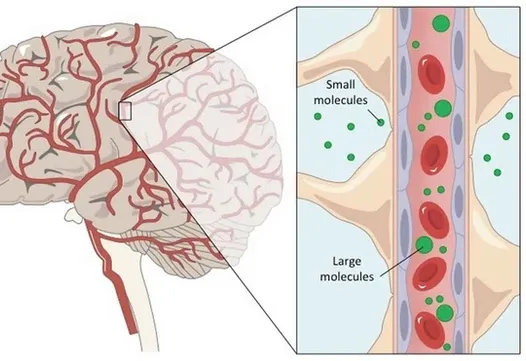
The brain is precious, and evolution has gone to great lengths to protect it from damage. The most obvious is our 7mm thick skull, but the brain is also surrounded by other protective mechanisms.
One important protective element is the blood–brain barrier. The blood-brain barrier is a thin lining that surrounds the brain and is designed to allow only nano-sized particles in or out as needed. As the name suggests, this is a barrier between the brain’s blood vessels (capillaries) and the cells and other components that make up brain tissue. Whereas the skull, meninges and cerebrospinal fluid protect against physical damage, the blood–brain barrier provides a defense against disease-causing pathogens and toxins that may be present in our blood.
However, like the gut, it can become damaged and “leaky,” allowing foreign invaders in. One of the biggest risks to triggering brain inflammation is a leaky blood-brain barrier.
HOW DOES A TBI CAUSE NEUROINFLAMMATION?
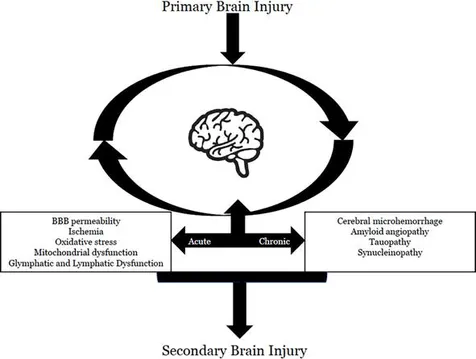
A traumatic brain injury (TBI) creates a cycle of neuroinflammation that can lead to secondary injuries and symptoms.
This is a brief overview of the neuroinflammatory cascade following a TBI:
LEAKY GUT SYNDROME AND NEUROINFLAMMATION
A typical human body is designed to take in a variety of foods, which are sent through different parts of the gastrointestinal system (i.e. digestive system) to be processed and converted into energy. Beneficial nutrients are absorbed and sent to the rest of the body for nourishment, while harmful components (toxins) are filtered out and excreted.
But what happens if the lining of the gastrointestinal tract or stomach is damaged, causing harmful toxins to enter the bloodstream? This is what we call Leaky Gut Syndrome (or intestinal permeability), and it is quite common after brain injuries.
With Leaky Gut Syndrome, undigested food particles cross into the bloodstream, resulting in inflammation and impaired nutrient absorption.
These undigested particles trigger a severe immune reaction, as the immune system sends signaling molecules and cytokines to the area, resulting in inflammation. Perhaps the most troubling part of Leaky Gut is that these cytokines are even capable of crossing the blood-brain barrier, which can cause inflammation in the brain–what we call neuroinflammation.
When the brain becomes inflamed, there is a drastic reduction in brain activity and this can majorly limit one’s ability to recover from a TBI, stroke, or concussion. This even has an impact on the gut-brain connection, which can create further issues in digestion. Basically, it is a loop of inflammation that needs to be broken.
Healing the gut lining becomes a top priority in this case, and resources like Cavin Balaster’s How To Feed A Brain can help along with your doctor’s recommendations.
REDUCING NEUROINFLAMMATION AND RESTORING THE BLOOD-BRAIN BARRIER
Because neuroinflammation occurs at acute and chronic stages after the primary insult in TBI, a treatment targeting neuroinflammation may have a wider therapeutic window for TBI. We focus on ways of reducing inflammation and preventing further neuroinflammation through our therapies, IV treatments, and nutritional guidance.
Although the blood-brain barrier degrades easily, it can also regenerate through dietary and lifestyle modifications similar to how you can repair leaky gut. For instance, high stress degrades the blood-brain barrier, but normalizing stress can allow it to repair. Simply stabilizing your blood sugar and stress levels, removing inflammatory foods, addressing chronic health issues, and taking powerful antioxidants can help restore the blood-brain barrier.
Common symptoms of neuroinflammation:
Supplements/herbs known to reduce neuroinflammation:
To learn more and become a patient at Resiliency, please fill out this contact form.
Research: